Members
Our service-first promise doesn’t stop with employers, brokers, and providers. With Concierge, you’ll have a clear understanding of your benefit offerings and a dedicated team here to assist you if a question does arise.
Our Commitment
Delivering responsive service is one of our core values here at Concierge because we understand how important the member experience is. That’s why our plans are designed to serve you through creative excellence and humility, providing you with better coverage and better outcomes.
Give us a call sometime—we’ll pick up.
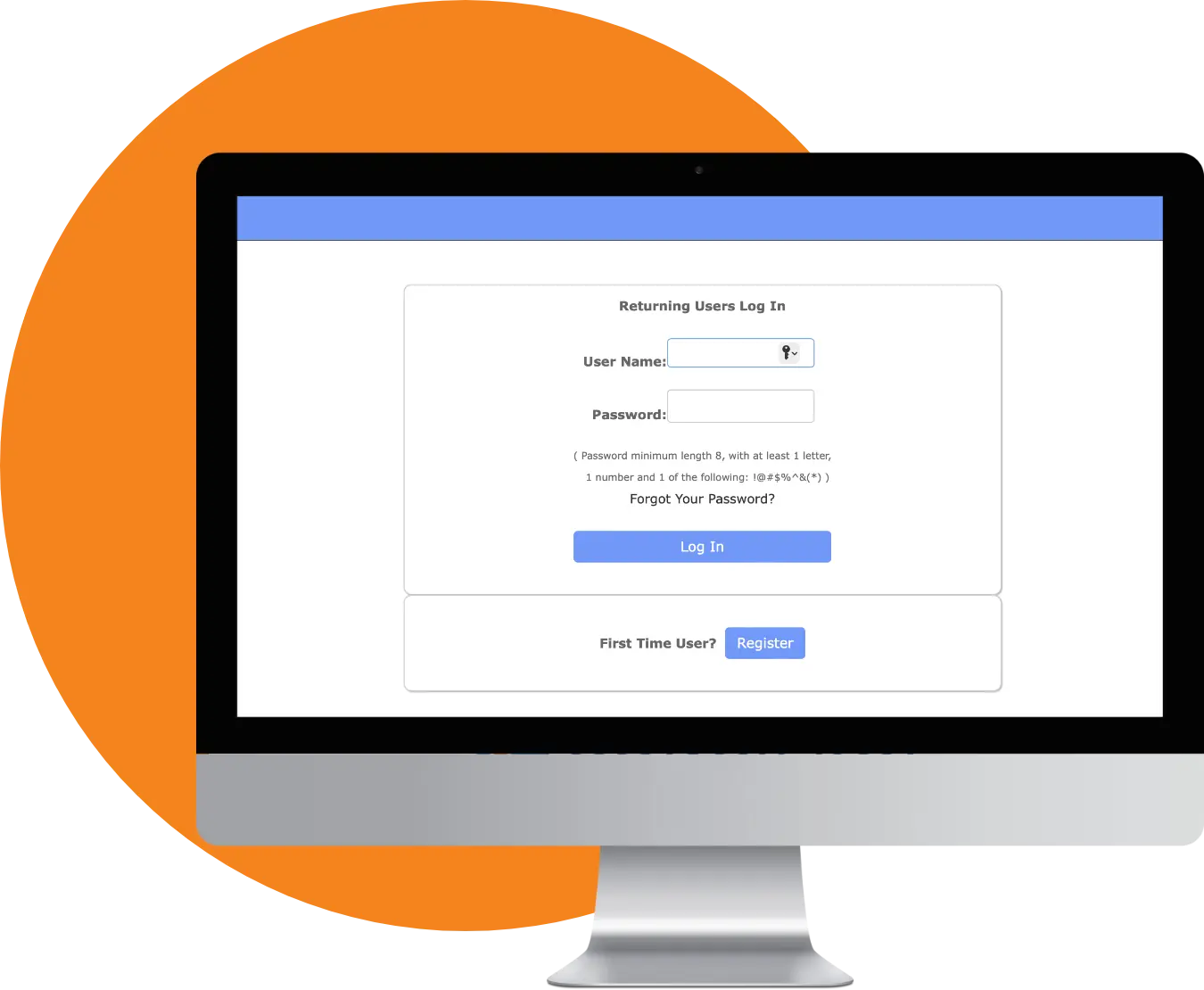
Member Portal
Our secure, easy-to-access member portal houses all important plan information while providing an avenue to receive direct support.
View your benefits
Access plan information
Contact customer service
File claims
Check claim status
Surprise Bills
You have rights and protections against surprise medical bills for certain out-of-network services. If you’re unsure of a bill you received or have a question about a doctor’s visit, give our team a call.
Member FAQs
Have a healthcare or coverage-related question? Our member-exclusive FAQ might have the answer!
Please reference your Employee Enrollment Guide for details about your benefits. If you do not have a copy of your Employee Enrollment Guide, please contact your employer to request a copy.
You’ll receive an electronic ID card from us via email or text! Once your coverage starts, you can print copies of your ID card or access them on your phone via the Clever Health app.
Clever Health provides smart virtual round-the-clock healthcare services. This gives our members access to board-certified providers, licensed therapists, and great care where and when they need it. Clever Health can include specialized veterinary services to help keep furry family members healthy, too.
You can text us directly at 918.876.5015 with any questions or concerns. Alternatively, you can call our team at 888.820.5687. If you’re requesting information, we’ll email or text you directly.
Go to your HealthWallet app to view your Summary of Benefits. For additional information, contact the Concierge customer service team at 888.820.5687.
You can view a list of participating network medical providers and their contact information in the Clever Health app under the PPO Network tab.
You can contact a virtual urgent care provider using the Clever Health app under ’virtual urgent care.’ If it is your first time requesting a consult, make sure to register by providing your personal information.
Yes! Each Concierge plan includes various preventative care services, which can all be found in your Employee Enrollment Guide. If you do not have a copy, please contact your employer.
EOBs are sent to members following a visit to a provider. An EOB is not a bill. It simply outlines the total charges for your visit as well as what was covered by your health plan.
The dental and vision benefits administered by Concierge do not require a network provider. Plan members may see any provider.
You can get your prescription coverage information through your plan’s portal and mobile application. You can also email us at eligibility@ctpa.com or text us at (918) 876-5015.
Need Further Assistance?
If you still have questions about claims, your coverage, or anything else, we’d love to help.
