Compliance: Cornerstone of Concierge
Concierge’s collaboration with WLT and TALON ensures adherence to the No Surprises Act (NSA), Consolidated Appropriations Act (CAA), and Transparency in Coverage (TiC) Rule. Benefits include but are not limited to the following:
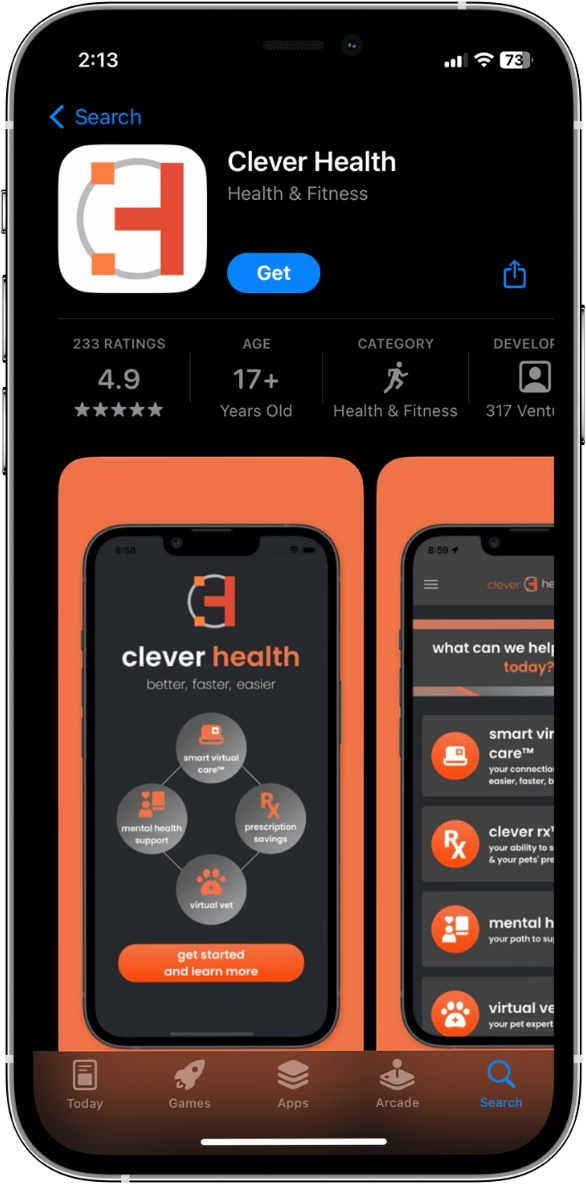
Members also enjoy the advantage of a dedicated portal to access more affordable healthcare options!
HSA and FSA Store
Through your health plan with Concierge, you may be eligible to enroll in a Health Savings Account (HSA) or Flexible Spending Account (FSA). Both types of accounts have dedicated online platforms, and each website offers a wide selection of qualifying products, making using healthcare funds simple. Click below to learn more and start shopping!
FAQs – The Answers You Need!
Need to Talk to us Directly Instead?
We’ve designed our FAQ section to answer the most common questions we receive. However, we know that each case and each person is different. If your question hasn’t been answered above, or if you need additional clarification on anything, we’re happy to help.