Providers
Our team values the role that providers play in the healthcare journey for our members, and we understand your time is valuable. We strive to deliver efficient claim administration and prompt payments to support patient care.
Empowering Better Health Outcomes
Delivering quality care to our members is a priority both for us and excellent providers like you! Our values guide and enable us to support you with access to real-time patient information, ensuring you can focus more on what matters—patient care.
Responsive Service
Answering the phone within 13 seconds, on average
Humility
Focusing on delivering for you, not ourselves
Creative Excellence
Crafting new ways to better serve you & our members
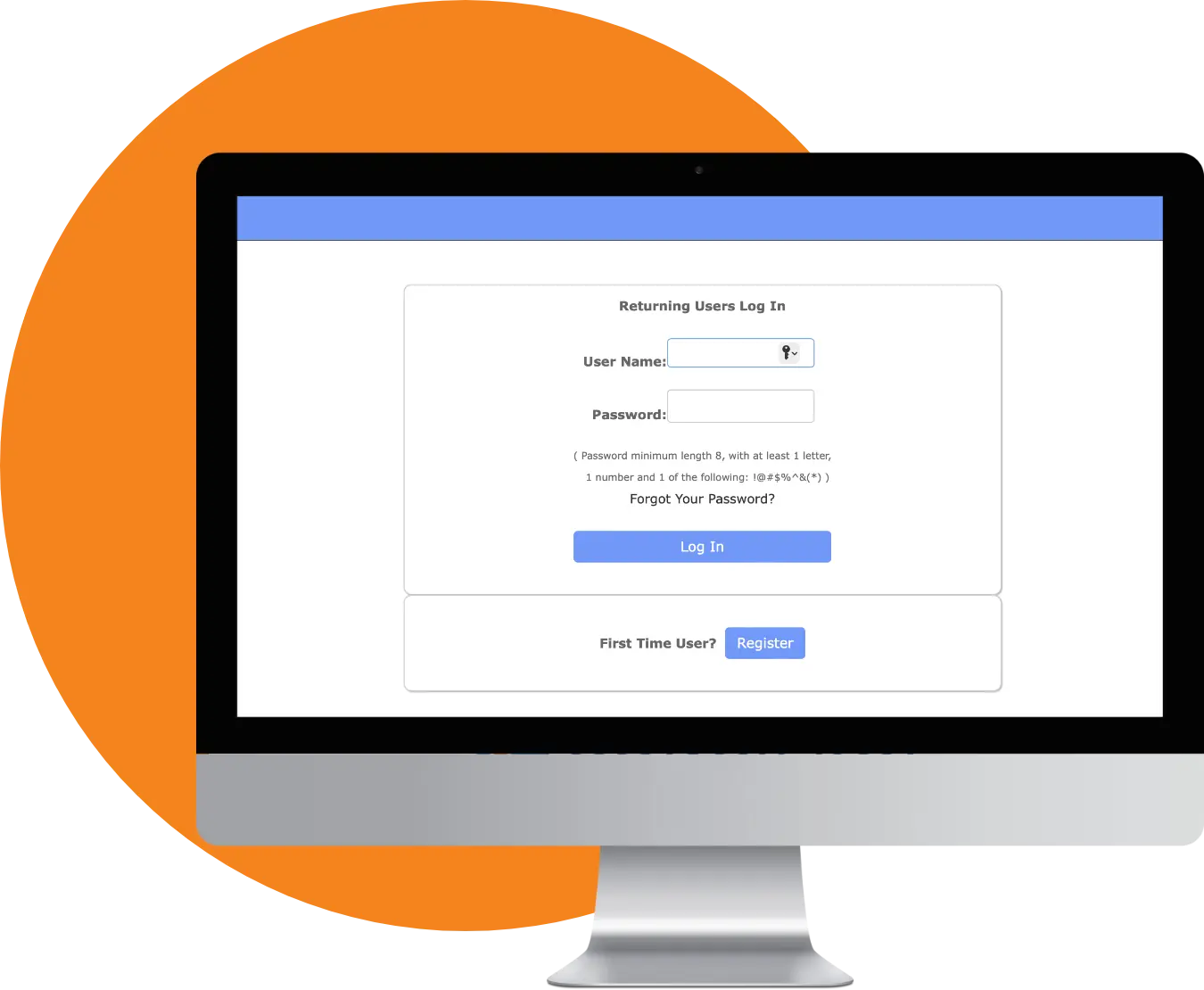
Welcome to Your
Provider Portal
Our Provider Portal is designed to support you with these resources:
Provider FAQs
We understand that not being able to access the Provider Portal is frustrating. Our team is here to help set things up correctly for you. Give us a call at 888.820.5687.
There are several reasons a patient’s information might not appear in your provider portal. Contact our team at 888.820.5687, and we’ll be happy to assist.
Send electronic claims to our Payer ID - CAS01. Paper claims should be sent to P.O. Box 4070, Bartlesville, Oklahoma 74006.
Send electronically to our Payer ID - CAS01. Paper requests should be sent to P.O. Box 4070, Bartlesville, Oklahoma 74006.
You can check member eligibility easily via the Provider Portal. You can also reference your digital ID Card on the HealthWallet mobile App. Call our customer service team at 888.820.5687 to check eligibility.
We have ACH available for provider payments. Please contact our team at 888.820.5687, to receive the form required to set it up.
Send it to: P.O. Box 4070, Bartlesville, Oklahoma 74006.
Yes, the appeal must be made within 180 days of the adverse benefit determination. If after careful review, it is determined that an error has been made, an additional payment may be made.
